Until recently stroke was a non-treatable disease – the management consisted of rehabilitation and prevention. Reversibility of this dreadful event was wishful thinking. But much has been happening over the last few years, and it is worth keeping up to date with the latest therapies.
Stroke is becoming a treatable condition
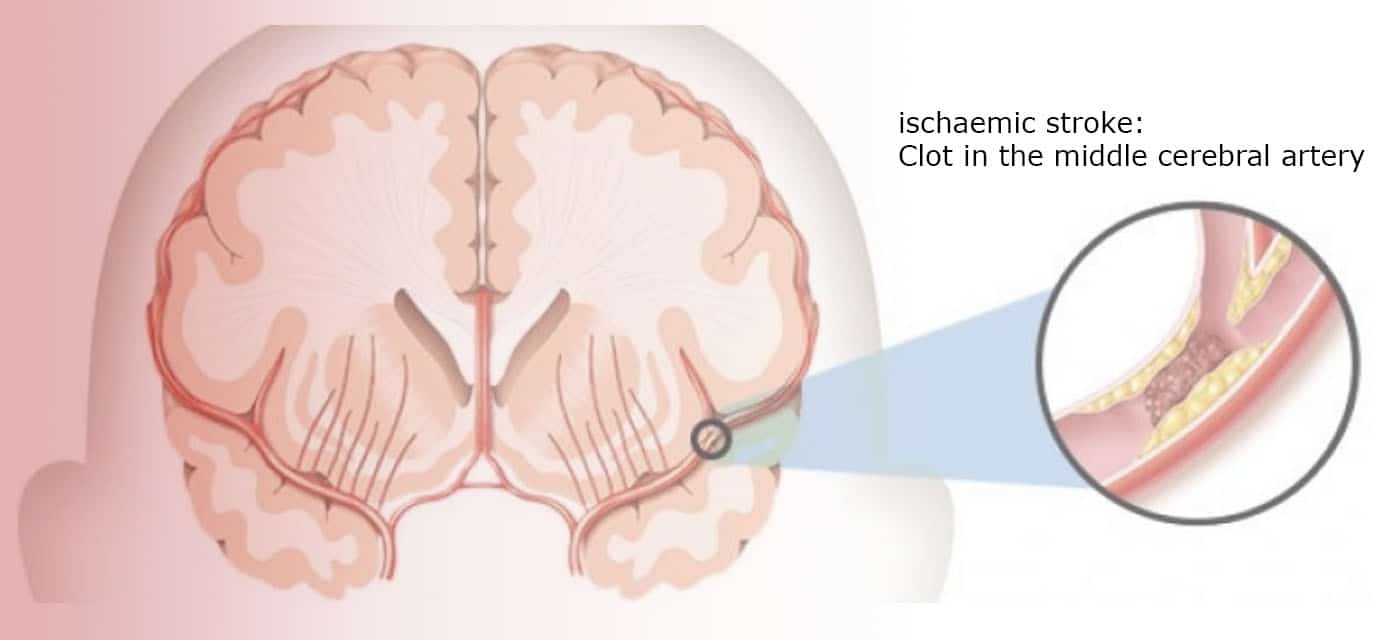
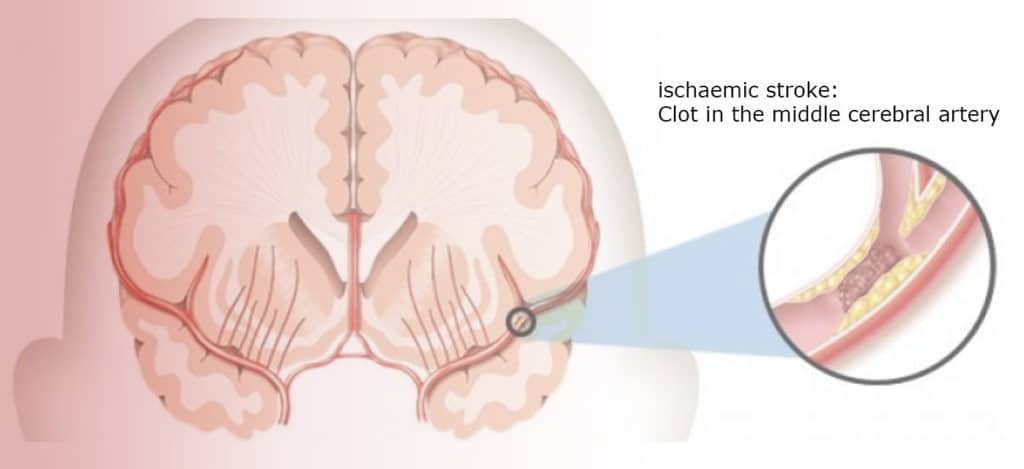
After the successful introduction of clot-busting therapies, where thrombus-dissolving agents are administered intravenously, we have now a mechanical option called thrombectomy available. This intra-arterial clot removing approach aims to physically remove the blood clot.
How does thrombectomy work?
Just like a coronary intervention, cerebral thrombectomy uses catheters that are inserted into a large artery to reach the area in the brain where the blockage occurs. And just like a coronary angiography, the procedure is performed by an interventional cardiologist – perhaps in the future renamed to neuro-cardiologist.
Time is of the essence
The aim is to quickly Identify the area where the obstruction occurs. This is done with a CT-scan which is urgently performed when a patient arrives at the emergency department. In order to be eligible for thrombectomy, the blocked vessel in question must fulfil specific criteria relating to its size and location. Only large vessel occlusion and currently just arteries of the anterior cerebral circulation are amenable to thrombectomy. Currently, the recommended time frame in which the clot is to be removed is 6 hours, keeping in mind that faster action delivers better results – Time is Brain.
The catheter is then inserted via the femoral artery to mechanically remove the thrombus.
What are the dangers?
Like all endovascular procedures, complications can be related to vessel injury caused by the device. These risks include perforation, dissection and bleeding. Adverse reactions may also be due to radiological contrast media.
What does the future hold?
The primary goal of this approach is rapid, safe and effective arterial recanalisation. If successful, the vital blood flow to the nerve tissue in the brain will be restored and brain damage kept to a minimum. Recent randomised clinical trials show that endovascular thrombectomy for large vessel ischaemic stroke has improved the outcome, leaving the stroke patient with less disability.
To become available for every future stroke patient, this new technology will demand interdisciplinary co-operation, and no doubt require huge organisational changes within the care provider. In the meantime, it is crucial that the public is aware of this new treatment and
A simple animation of this procedure can be seen at:
Patient education
Many Western healthcare providers are taking part in Public stroke education and are highlighting the importance of acting quickly. The “FAST” campaign has proved to be very successful in the UK and US to help recognise signs of a stroke; it uses the acronyms as follows:
• F: Face drooping
• A: Arm weakness
• S: Speech difficulty
• T: Time to call the emergency